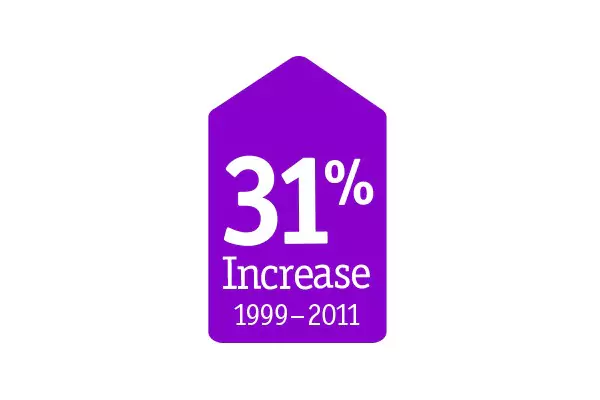
Calcium is more common than you think
In the United States, over 30% of all patients treated for PCI present with some degree of calcium. This represents a 31% increase over the last two decades alone. Patient complexity is increasing; risk factors such as an aging population, renal failure, hypertension, and an increasing prevalance of Type C lesions indicate that calcific lesions will continue to be present.1

Calcium can present complications
A range of complications can arise during a procedure, including: dissection during balloon angioplasty or pre-dilatation2, difficulty with complete dilation3, inhibition of adequate stent expansion4, prevention of stent delivery to the desired location5, stent under expansion or malapposition6, insufficient drug penetration and subsequent restenosis7.

Incomplete dilation2

Inadequate stent expansion4
Stent malapposition6
Calcium is a predictor of worse outcomes
Optimal treatment is necessary to improve long-term patient outcomes.
Moderate to severe calcium creates a significantly higher chance of complications like MI, TLR, MACE and death.8
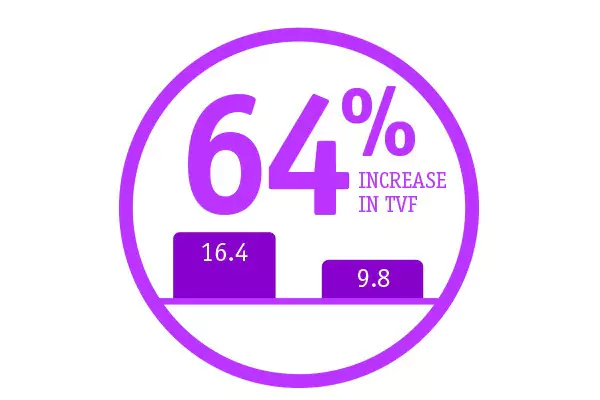
Target vessel failure is higher in cases with severe calcification. At two years, TVF was 16.4% for those with severe calcification vs. 9.8% than those without severe calcification.9